Medically Reviewed by: Scientific Advisory Board
We're all aware of the general complications that diabetes can cause, but often a less-discussed issue is diabetic foot ulcers. Affecting up to 25% of diabetics, these wounds on the feet can become a serious matter if not properly managed. As experts in the field, we aim to shed light on this topic to help prevent complications and improve the quality of life for those living with diabetes.
Living with diabetes presents numerous health-related challenges, and for some, proper foot care is crucial in maintaining well-being. Diabetic foot ulcers occur when a layer of skin breaks down, allowing bacteria to enter and potentially cause infections. If left untreated, these ulcers can lead to serious health issues and in extreme cases, may even result in amputation. That's why it's essential to understand their causes, as well as the best methods for prevention and treatment.

We'll be delving deeper into the subject of diabetic foot ulcers, touching on the various risk factors and causes, signs and symptoms to watch out for, and advice on how to effectively manage these distressing wounds.
Understanding a Diabetic Foot Ulcer
We're here to help you understand diabetic foot ulcers and why they can be a serious complication for individuals with diabetes. Diabetic foot ulcers are open sores or wounds that typically form on the bottom of the foot, which can develop in up to 15% of diabetes patients.
The risk factors for diabetic foot ulcers include:
- Neuropathy: Nerve damage in the feet can cause loss of sensation, making it difficult to notice injuries or pressure points.
- Peripheral Artery Disease (PAD): Reduced blood circulation to the feet prevents quick healing of wounds and can worsen existing ulcers.
- Deformities: Foot deformities, such as bunions or hammer toes, can cause irregular pressure distribution, leading to foot ulcers.
- Poorly fitting footwear: Shoes that are too tight or not well-cushioned can cause friction and pressure, contributing to ulcer formation.
| Risk Factor | Description |
|---|---|
| Neuropathy | Nerve damage in the feet, causing loss of sensation of injuries or pressure points |
| Peripheral Artery Disease | Reduced blood circulation, preventing quick healing of wounds and worsening ulcers |
| Deformities | Foot deformities causing irregular pressure distribution, leading to foot ulcers |
| Poorly fitting footwear | Shoes causing friction and pressure, contributing to ulcer formation |
Prevention is crucial in reducing the risk of diabetic foot ulcers. We suggest taking the following steps regularly:
- Check your feet daily for any changes or injuries
- Keep your feet clean and dry to avoid infections
- Wear well-fitting, comfortable shoes, and consider using diabetic socks
- Moisturize your feet to prevent dryness and cracking
- Trim your toenails regularly to avoid injury
- Maintain good blood glucose control to reduce the risk of nerve damage and poor circulation
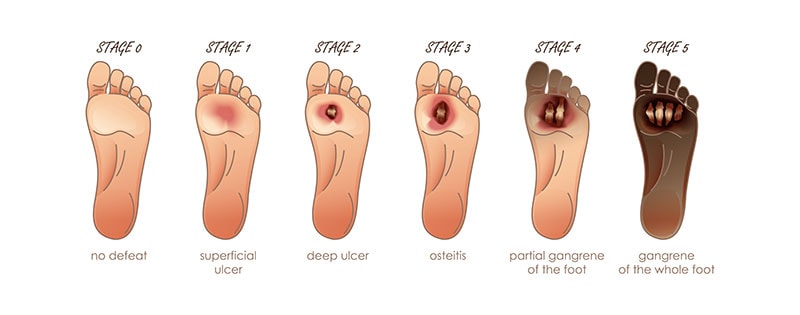
Understanding the stages of diabetic foot ulcers helps provide insight into their severity:
- Stage 1: Redness and swelling, often accompanied by pain or discomfort
- Stage 2: Breakdown of the skin, forming an open wound
- Stage 3: Deepening of the wound, potentially involving muscles or tendons
- Stage 4: Spread of infection to surrounding tissue and bones
Prompt treatment of diabetic foot ulcers is crucial in preventing infection and minimizing the risk of amputation:
- Regular wound cleaning with proper dressings
- Offloading pressure from the ulcer through the use of specialized footwear or devices
- Addressing infection through antibiotics
- Ensuring proper blood flow to the affected area through vascular procedures if needed
By understanding the risk factors, prevention methods, and treatment options for diabetic foot ulcers, we're better equipped to manage this complication and maintain good foot health. Remember that timely intervention plays a key role in successful treatment, so always consult your healthcare professional if you notice any signs of a developing foot ulcer.
Causes and Risk Factors for Diabetic Foot Ulcers
Understanding the causes and risk factors for diabetic foot ulcers is crucial in helping us manage and prevent these painful wounds. Diabetic patients are at a higher risk for developing foot ulcers due to several factors.
The primary cause of foot ulcers in diabetic patients is neuropathy. Over time, diabetes can damage the nerves, making it difficult for patients to feel pain or discomfort. This increases the likelihood of developing ulcers as unnoticed injuries and pressure may cause skin breakdown.
Poor blood circulation is another significant factor contributing to ulcer development. Diabetes often affects blood vessels, leading to vascular diseases which further reduce blood flow to the extremities. Inadequate blood circulation reduces the body's ability to heal wounds and fight infections, making it easier for ulcers to form.
Foot deformities like bunions, hammertoes, and Charcot arthropathy make it more challenging for diabetic patients to find proper footwear, increasing pressure on certain areas of the foot and consequently raising the risk of ulcers.
Additional risk factors that exacerbate the likelihood of diabetic foot ulcers are:
- Long-term diabetes: The longer a person has diabetes, the greater the chances of peripheral neuropathy and vascular diseases.
- Uncontrolled blood sugar levels: Poorly managed diabetes can result in more extensive nerve damage, reducing the body's ability to heal and increasing the risk of ulcers.
- Obesity: Being overweight puts undue pressure on the feet, exacerbating potential skin breakdown and ulcers.
- Smoking: Smoking disrupts blood circulation and hampers wound healing, making it a significant risk factor for ulcers.
Taking care of our feet is essential to prevent the development of diabetic foot ulcers. Being aware of these risk factors can help us make informed decisions to lower our chances of experiencing ulcers and their devastating effects. Regular foot checks, wearing appropriate footwear, and managing blood sugar levels can significantly improve the overall foot health of diabetic patients. Our knowledge and preventive measures make a difference in maintaining our well-being and avoiding diabetic foot ulcers.
Common Symptoms and Complications
Diabetic foot ulcers can cause significant discomfort and may lead to serious complications. We'd like to discuss some of the most common symptoms and complications, helping you recognize issues and seek prompt medical attention.
A primary symptom of a diabetic foot ulcer is the presence of an open sore or wound on the foot. This wound might ooze fluid or develop a foul smell. Other common symptoms include:
- Swelling around the ulcer
- Discoloration of the skin, turning red, brown, or black
- Pain in the area surrounding the ulcer
It's crucial to attend to these symptoms, as ignoring them might result in complications. The following are some of the most common and serious complications associated with diabetic foot ulcers:
-
Infections: Diabetic foot ulcers are prone to bacterial infections. If an infection occurs, you may notice increased redness, pus discharge, or a foul smell. Left untreated, infections can spread through the tissues or even into the bloodstream, potentially causing life-threatening sepsis.
-
Gangrene: Severe cases of infection or poor blood flow can lead to tissue death, aka gangrene. This condition is indicated by the skin turning black or blue and requires urgent medical care. In some cases, amputation may be necessary to prevent further tissue damage or spreading of the infection.
-
Bone infections (osteomyelitis): When an infection originating from a foot ulcer spreads deeper, it can affect the bones, necessitating a prolonged course of antibiotics or surgery to remove the infected bone.
-
Charcot foot: Damage to the nerves and blood vessels in the foot can weaken bones and joints, resulting in a condition known as Charcot foot. Symptoms include swelling, warmth, and redness, often with no apparent injury. If left untreated, it can lead to severe deformities and functional impairment.
To minimize these complications, proactive steps include:
- Monitoring foot health regularly for changes or signs of ulcers
- Maintaining good blood sugar control
- Proper foot hygiene, such as washing and drying your feet regularly
- Wearing specially designed diabetic socks to help prevent ulcers by providing moisture-wicking properties and gentle compression to enhance blood flow
Taking these steps and seeking medical attention when symptoms arise can significantly reduce the detrimental effects of diabetic foot ulcers and improve overall quality of life.
Diagnosis and Treatment Options
Diagnosing a diabetic foot ulcer starts with a thorough examination by a healthcare professional. They'll assess the wound's depth, size, and location, and check for infections. We're going to cover some common diagnostic tests and treatment options to help you better understand the process.
During the diagnosis, a few tests might be performed, such as:
- Swab culture: helps identify any bacteria present in the ulcer.
- Blood tests: may reveal elevated levels of inflammatory markers, indicating infection.
- X-ray or MRI: can detect any underlying bone injury or osteomyelitis (bone infection).
The primary aims of diabetic foot ulcer treatment include:
- Managing the infection through antibiotics, prescribed according to the identified bacteria.
- Debridement, removing dead tissue and calluses from the ulcer, promoting healing and preventing further infection.
- Employing offloading techniques such as customized footwear, walking casts, or crutches to redistribute pressure and relieve the affected area.
We'd like to share some other significant treatment options:
- Wound dressings: keeping the ulcer clean and moist with proper dressings, as suggested by a healthcare professional, is crucial.
- Negative pressure wound therapy (NPWT): involves application of controlled suction to the area, promoting healing by removing excess fluids and stimulating tissue growth.
- Hyperbaric oxygen therapy (HBOT): patients breathe 100% oxygen in a pressurized chamber, thereby improving the oxygen supply to the affected tissues and promoting wound healing.
- Growth factor therapy: applying growth factors directly to the ulcer to expedite the healing process.
| Type | Description | Usefulness |
|---|---|---|
| Antibiotics | Drugs prescribed to combat infection | Essential for infected ulcers |
| Debridement | Removing dead tissue from the affected area | Promotes wound healing |
| Offloading techniques | Redistributing pressure away from the ulcer | Aids in healing and pain relief |
| Wound dressings | Protective coverings for the ulcer | Encourages a moist healing environment |
| NPWT | Application of suction to the wound area | Contributes to healing and tissue growth |
| HBOT | 100% oxygen in a pressurized chamber | Improves oxygen supply in affected area |
| Growth factor therapy | Applying growth factors directly to the ulcer | Hastens the healing process |
In conclusion, proper diagnosis and treatment are imperative in the successful management of diabetic foot ulcers. By selecting appropriate treatments and following healthcare professionals' advice, we can help prevent complications and ensure a faster recovery.
Prevention Strategies and Self-Care
An essential part of managing diabetes is preventing diabetic foot ulcers (DFUs). We'll discuss a few prevention strategies and self-care tips that can help reduce the risk of developing DFUs.
Proper foot care is crucial for those with diabetes. Here are some vital steps to take:
- Inspect your feet daily for cuts, blisters, redness, or swelling. Early detection enables timely treatment and reduces the risk of complications.
- Wash your feet with mild soap and warm water every day. Dry them thoroughly, paying particular attention to the areas between the toes.
- Moisturize your feet to avoid dry skin, which may lead to cracks and potential infections. Avoid applying moisturizer between the toes since excess moistness can promote fungal growth.
Protecting your feet from injury is equally important. Consider the following recommendations:
- Wear properly fitted shoes that provide ample support and cushioning. Avoid tight, ill-fitting shoes that can cause pressure sores, blisters, or cuts.
- Rotate your footwear to allow for proper drying and discourage bacterial growth.
- Avoid walking barefoot both indoors and outdoors to minimize the risk of cuts, punctures, or burns.
In addition to foot care and protection, it's essential to maintain healthy blood sugar levels since high glucose levels impair wound healing. Implement these strategies:
- Monitor your blood sugar regularly and follow your doctor's advice for maintaining optimum levels.
- Stick to a healthy diet that's low in saturated fats, sugars, and refined carbohydrates. Include more fresh fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Stay active by engaging in regular physical activity, such as walking, swimming, or biking, with your doctor's approval.
Let's not forget the importance of regularly scheduling appointments with your healthcare team:
- Have a comprehensive foot exam at least once a year, or more frequently if recommended by your doctor.
- Promptly report any foot-related concerns or changes to your healthcare team. Early intervention is critical for preventing complications.
Wearing specialized footwear, such as diabetic socks, can also help prevent DFUs. Diabetic socks offer medically proven benefits and ensure maximum comfort for people with diabetes.
By following these prevention strategies and self-care guidelines, together we can reduce the risk of diabetic foot ulcers and support healthy feet for a better quality of life.
Wrapping Up Our Insights
Throughout this article, we've explored the complex and potentially life-changing subject of diabetic foot ulcers. By understanding the causes, symptoms, and preventative measures, individuals with diabetes can take control and improve the quality of their lives. In this final section, let's briefly recap the essential points we've covered.
- Diabetic foot ulcers are open sores that develop on the feet of individuals with diabetes, and they're a common complication caused by several factors like poor blood circulation and neuropathy.
- Early detection and treatment of diabetic foot ulcers are crucial in preventing complications like infection and amputation.
- To avoid diabetic foot ulcers, we advise implementing the following practices:
- Inspecting your feet daily for any signs of injury or infection
- Washing your feet with warm water and soap, and moisturizing regularly
- Wearing the right footwear designed for diabetic individuals, such as medical-grade socks with Circufiber™ technology
- Scheduling regular check-ups with a healthcare professional
It's essential to recognize that we all have a role to play in managing our health, and by staying informed and making smart choices, we can work together to mitigate the risks associated with diabetes. If you or a loved one is living with diabetes, take the time to educate yourself on diabetic foot ulcers and other potential complications. Armed with knowledge, support, and the right resources, we can maintain our well-being and face the challenges of diabetes head-on.
References, Studies and Sources:
https://www.ncbi.nlm.nih.gov/books/NBK537328/
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.