We're here to guide you through the creation of your own personalized diabetes exercise plan. Understanding how physical activity affects blood sugar levels is essential for anyone living with diabetes.
Exercise plays a significant role in maintaining healthy blood glucose levels because it aids insulin effectiveness. Regular movement can also help us manage our weight, reduce stress, and increase our overall fitness level. But initiating an effective fitness regimen isn't always straightforward when you're managing diabetes.
Whether you're new to regular exercise or looking to enhance your current routine, we'll help navigate the ins and outs of exercising with diabetes.
Understanding the Importance of Exercise in Diabetes Management
Exercise plays a pivotal role in managing diabetes. It's not just about staying fit or losing weight, it's about maintaining a balance that your body needs to function properly. Regular physical activity can help regulate blood sugar levels, which is crucial for people living with this condition.
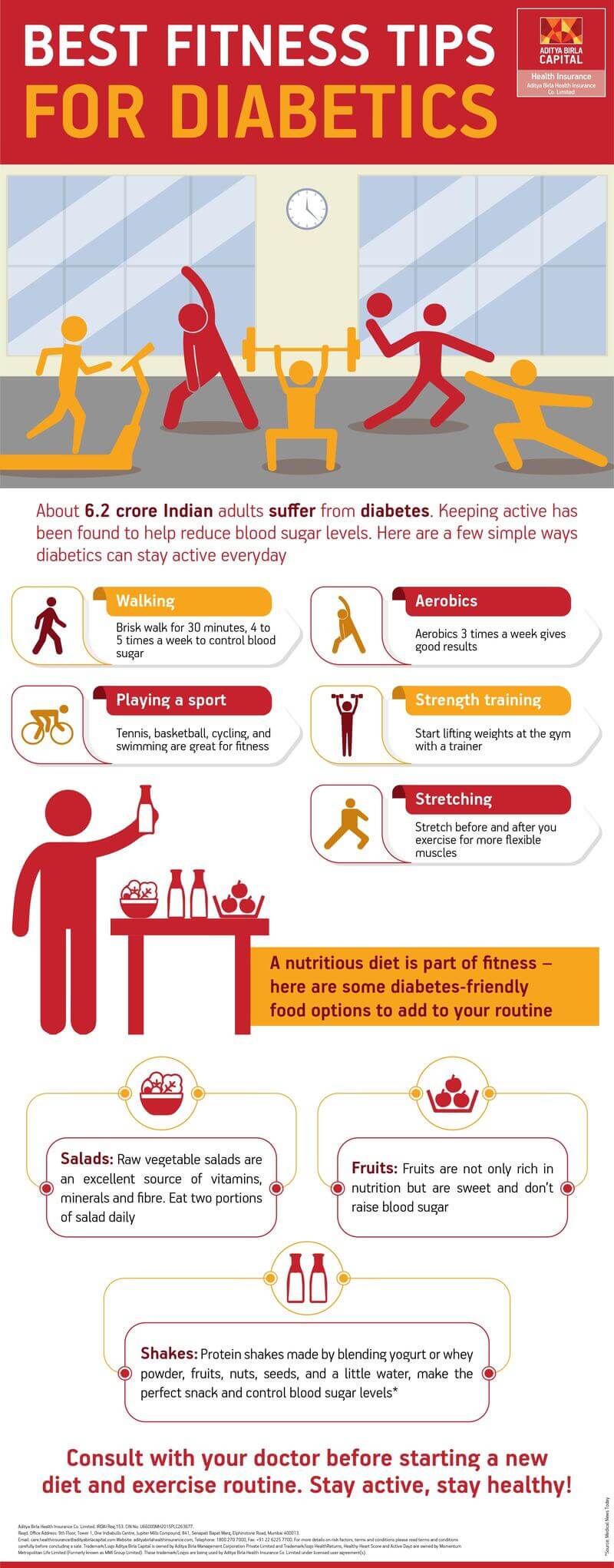
According to the American Diabetes Association, adults with diabetes should aim for at least 150 minutes of moderate-to-vigorous intensity aerobic exercise each week. This could include activities such as walking briskly, cycling or swimming.
| Activity | Intensity | Duration |
|---|---|---|
| Walking | Moderate | 30 mins/day |
| Cycling | Moderate | 30 mins/day |
| Swimming | High | 20 mins/day |
These numbers aren't set in stone and it's important to remember that any increase in physical activity can have positive effects on blood glucose control. We're all unique, so what works for one person might not work for another. It's essential to find an exercise routine that suits you and aligns with your lifestyle.
Exercise also has additional health benefits for those with diabetes. It improves cardiovascular health - reducing the risk of heart disease which is high among diabetics. Moreover, regular workouts improve mental wellbeing by reducing stress and anxiety levels – two factors known to exacerbate diabetic symptoms.
Always consult with healthcare professionals before starting any new fitness regimen if you are living with a chronic illness like diabetes.
Creating a Personalized Diabetes Exercise Plan
Crafting an exercise plan tailored to your needs can be a powerful tool in managing diabetes. It's not just about the type of activity, but also the intensity and timing that play crucial roles in glucose control.
The first step is understanding your body. We all have different fitness levels and health conditions. Therefore, it's necessary to consult with healthcare professionals before starting any new exercise regimen. They can help evaluate your current fitness level and guide you on how to progressively increase the intensity of workouts without risking hypoglycemia (low blood sugar).
Next, consider your interests and lifestyle when choosing activities for your exercise plan. Engaging in physical activities you enjoy will boost motivation and adherence over time. Options could include walking, cycling, swimming, or strength training - all great choices for people with diabetes.
It's equally essential to pay attention to timing. Since exercise affects blood sugar levels for several hours afterward, scheduling workouts around meal times can help manage glucose fluctuations effectively.
Here are some general guidelines based on American Diabetes Association recommendations:
- Aim for 150 minutes of moderate-intensity aerobic activity per week spread over at least three days.
- Avoid going more than two consecutive days without physical activity.
- Include resistance training at least twice a week.
Lastly, remember that consistency is key. Even small bouts of movement throughout the day add up and contribute significantly towards achieving optimal health goals.
Safety Measures for Physical Activity with Diabetes
Engaging in regular physical activity is a crucial component of managing diabetes. However, there are certain safety measures we must take into consideration when creating an exercise plan.
Firstly, it's essential to monitor blood glucose levels before and after exercising. Physical activity can affect these levels significantly, so understanding how exercise impacts your body allows you to better manage your diabetes. It might be helpful to keep a log of your readings to identify patterns or trends over time.
In addition, staying hydrated during workouts is equally important. Dehydration can lead to high blood sugar levels and even increase the risk of diabetic ketoacidosis (DKA), particularly in individuals with type 1 diabetes. So always remember to drink water before, during and after exercise.
Next on our list is the importance of proper foot care. People living with diabetes often have nerve damage in their feet which makes them more susceptible to injuries or infections that they may not feel due to lost sensation. Therefore, wearing comfortable and protective footwear during workouts is paramount.
Here's a quick rundown:
- Regular monitoring of blood glucose levels
- Staying well-hydrated
- Taking good care of the feet
It's also crucial that you don't push yourself too hard initially when starting new exercises or routines - gradual progression is key here. If at any point you feel dizzy or lightheaded during exercise, stop immediately and seek medical attention if necessary. Finally, always consult with your healthcare provider before starting any new workout regimen - they'll be able to offer personalized advice based on your current health status and goals. This way we can ensure a safe yet effective approach towards physical activity amidst living with diabetes.
Adapting Your Diet for Your Diabetes Exercise Routine
When we're working towards a healthier lifestyle, it's not just the exercise that matters. What we eat plays a pivotal role too, especially when managing diabetes. Let's delve into how you can adapt your diet to complement your exercise routine.
To start off with, it's crucial to understand how food affects our blood sugar levels. Every time we eat, our body breaks down carbohydrates into sugars which enter our bloodstream. This prompts the pancreas to release insulin that helps absorb these sugars and use them for energy. However, if you have diabetes, this process doesn't work as effectively leading to higher blood sugar levels.
Maintaining a consistent eating schedule is key in managing blood sugar levels during exercise. Regular meal times aligned with your workout schedule can prevent low or high blood sugar episodes. It’s also wise to include snacks before and after workouts if needed.
When crafting your meals and snacks around workouts, focus on including complex carbohydrates like whole grains, fruits and vegetables alongside lean proteins such as chicken or tofu. These foods provide sustained energy without causing sudden spikes in blood sugar levels.
- Pre-workout: A small snack 30 minutes before exercising can give you the boost of energy you need while preventing low blood sugar.
- During workout: If your session lasts more than an hour consider having a carb-rich snack like half a banana or few raisins.
- Post-workout: To replenish spent glycogen stores have some protein paired with carbs within 45 minutes after finishing your session.
Remember creating an effective diet plan around your exercise regimen isn’t about drastic changes but rather about balance and consistency over time which will help manage diabetes better while keeping us energized for those all-important workouts.
Conclusion: The Long-Term Benefits of an Effective Diabetes Exercise Plan
Regular physical activity plays a crucial role in managing diabetes, and it's one piece of the puzzle you don't want to overlook.
Firstly, consistent exercise helps regulate blood sugar levels. It enhances your body's sensitivity to insulin, which is essential for controlling glucose levels. Over time, this can reduce the need for medication and even help prevent complications associated with diabetes.
Secondly, regular workouts contribute towards weight management. Maintaining a healthy weight is vital for overall health and particularly important for individuals living with diabetes. Obesity or being overweight can exacerbate symptoms and make it harder to manage the condition.
Thirdly, exercise boosts heart health – another critical factor since people with diabetes are at higher risk for heart disease. Regular workout improves cardiovascular fitness by strengthening your heart muscle and promoting better circulation.
Finally, exercise enhances mental well-being too! It reduces stress levels and can improve mood – factors that shouldn't be underestimated when managing a chronic illness like diabetes.
We've tackled the topic thoroughly but remember that each person's journey with diabetes is unique. Stay informed, stay active, check in regularly with your healthcare team – these are all steps towards living well with diabetes.
References, Studies and Sources:
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.




