Medically Reviewed by:Scientific Advisory Board
When it comes to diabetes management, there's a lot we need to understand. We're dealing with a complex condition that affects millions of people each day, and while it's not always easy, it's far from impossible. Knowledge, after all, is key in tackling this health issue head on.

Living with diabetes doesn't mean you can't enjoy life to the fullest. It requires regular monitoring of blood sugar levels and maintaining a balanced diet and exercise routine but these are manageable tasks once you get the hang of them. We'll help guide you through your journey, offering tips and advice based on scientific research.
We have to remember that every person's body reacts differently to food, exercise, stress, medication and so on; what works for one might not work for another. That's why individualized care is vital in managing diabetes effectively. Together, we will explore various strategies that can be customized according to your lifestyle needs.
Understanding Diabetes Management
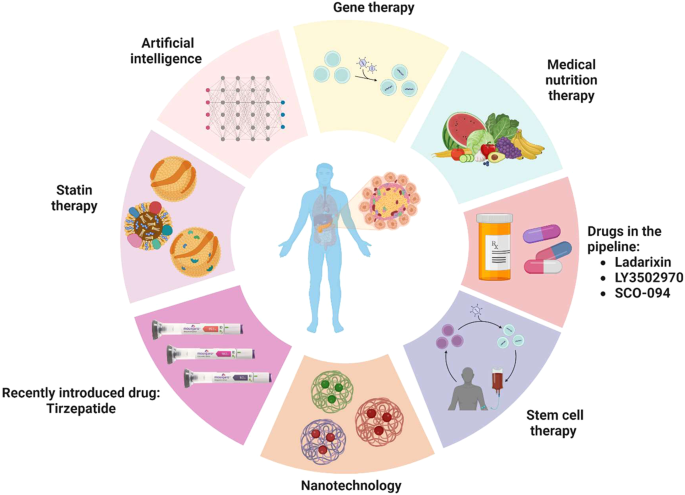
Diabetes management is an ongoing process that demands attention and commitment. When we have diabetes, we need to make daily decisions about what to eat, when to exercise, and how much medication to take.
Taking charge of our blood glucose levels is a key part of managing diabetes. Regular monitoring helps us see the impact of our choices on these levels. For instance, we might notice that after eating certain foods or doing specific exercises, our glucose levels fluctuate. Such insights can help us fine-tune our approach towards maintaining healthy glucose levels in our bloodstream.
Maintaining a balanced diet is another crucial aspect of diabetes management. We're not just talking about cutting out sugar here. A well-rounded diet includes a good mix of proteins, carbohydrates, and fats in appropriate portions for each meal.
Physical activity plays a vital role too. Regular exercise helps lower blood sugar levels and boosts insulin sensitivity - which means your body uses insulin more efficiently.
Medication also forms an integral part of the picture. Depending on the type and severity of our diabetes, we may need oral medications or insulin injections to manage blood sugar levels effectively.
In short: understanding diabetes management is all about balancing food intake with physical activity while keeping track of your medication regimen – it's like juggling balls in the air but with practice and patience, you'll get there. Remember – it’s not just about managing symptoms; it's also about preventing complications down the line.
Here are some key points:
- Monitoring blood glucose regularly.
- Following a balanced meal plan.
- Engaging in regular physical activities.
- Taking prescribed medications as directed by healthcare providers.
In essence, effective diabetes management hinges upon incorporating healthy habits into our everyday routines. After all - consistency is key when it comes to controlling this chronic condition.
The Role of Diet in Managing Diabetes
We can't stress enough how critical diet is when it comes to managing diabetes. It's a fundamental part of your routine, one that requires careful consideration and planning. It's not just about what you eat, but also when and how much.
First off, let's talk about carbs. They're often vilified in the world of dieting, but they're essential for our bodies. In the case of diabetes management, it’s all about controlling their intake. Consuming too many carbohydrates at once can spike blood sugar levels drastically which isn't ideal if you have diabetes. Therefore, understanding the concept of carb counting becomes crucial.
Now onto proteins and fats. These aren’t directly related to blood sugar levels but they play a role nonetheless:
- Proteins: While protein doesn’t directly affect blood sugars as much as carbs do, it does contribute to satiety—feeling full after eating—which can indirectly help control your overall calorie and carbohydrate intake.
- Fats: Healthy fats are an important part of any balanced meal plan although too much fat or the wrong type (saturated or trans fat) can lead to weight gain and other health problems.
Another key aspect we need to touch on is portion sizes. Controlling portion sizes helps maintain balance in your meals while preventing overeating which could cause spikes in blood sugar levels.
Lastly, consistency is key. Regular meal times paired with consistent carbohydrate intake will help keep your glucose levels steady throughout the day.
In essence managing diabetes through diet isn't about deprivation – it's more about making smarter choices that work best for you. Keep these pointers in mind as you navigate through this journey towards better health with diabetes.
Exercise Strategies for Diabetes Control
Active management of diabetes is crucial and exercise plays a key role in this. Regular physical activity can help control blood sugar levels, lower your risk of heart disease, and improve overall mental health. So let's dive into some effective strategies to incorporate exercise into your diabetes management.
Aiming for at least 30 minutes of moderate-intensity exercise five days a week is a good place to start. This might include brisk walking, swimming or cycling. It's important to remember that every bit counts and even short bursts of activity throughout the day add up. For instance:
- Parking further away from the store entrance
- Taking the stairs instead of the elevator
- Walking during lunch breaks
Strength training also holds significant benefits for people with diabetes. By building muscle mass, we increase our body's ability to regulate glucose. Activities like weightlifting or yoga can be incorporated two or three times a week.
Maintaining consistency is key when it comes to exercising with diabetes. Regular workouts help your body use insulin more effectively and keep blood sugar stable over time.
Monitoring blood sugar before and after workouts becomes essential too. If you notice your levels are too low post-exercise, having a small snack beforehand can prevent hypoglycemia.
Getting started with an exercise regimen may seem daunting but remember, it doesn't have to happen all at once. We recommend starting slow and gradually increasing intensity as you become more comfortable.
Lastly, always consult with healthcare professionals before making changes to your fitness routine — they can provide personalized advice based on your unique health situation.
Incorporating these strategies will not only assist in controlling diabetes but will also contribute positively towards overall wellbeing.
Medication and Monitoring: Key Aspects of Diabetes Management
Effectively managing diabetes is a balancing act. It's about keeping blood sugar levels within the target range set by healthcare professionals. One of the cornerstones of this management is medication, while another equally crucial aspect is regular monitoring.
Medications play an essential role in diabetes management. They're designed to help our bodies either use insulin more efficiently or make more insulin. For those with Type 1 diabetes, it's typically insulin injections to replace what their body can't produce. The story might be different for people with Type 2 diabetes - they could be prescribed oral medications or non-insulin injectables that encourage their own bodies to produce more insulin.
Monitoring blood glucose levels, on the other hand, provides a real-time snapshot of how well we're managing our condition. Most individuals measure their blood sugar several times a day using a glucose meter or continuous glucose monitor (CGM). This data not only helps us understand how food, exercise, stress, and medications affect our blood sugar but also guides any necessary adjustments to keep things optimal.
To highlight just how significant these two aspects are in managing diabetes:
| Aspect | Importance |
|---|---|
| Medication | Helps regulate blood sugar levels by increasing insulin efficiency or production |
| Monitoring | Provides crucial real-time data on current blood glucose level |
We also need to remember that every individual's journey with diabetes is unique - what works wonders for one person may not have the same impact on others. Therefore it's absolutely vital that all treatment plans and management strategies are personalized under professional guidance.
While medication and monitoring lay the foundation for effective diabetes control, they intertwine with various other elements like diet and exercise - painting the bigger picture of comprehensive self-care in living successfully with this condition.
Conclusion: Embracing a Healthy Lifestyle for Diabetes Management
Embracing a healthy lifestyle is fundamental to diabetes management. It might seem challenging at first, but trust us when we say that it's possible and incredibly rewarding.
It's essential to maintain a balanced diet. Foods rich in fiber, lean proteins, fruits and vegetables should become your best allies. Junk food? Let's keep that as an occasional treat rather than the norm.
Don't forget about exercise either. Physical activity not only helps control blood sugar levels but also boosts your overall wellbeing. Whether it's brisk walking, swimming or yoga – find something you love doing and stick with it.
Regular monitoring of blood glucose levels is another crucial aspect of diabetes management. This way, we can spot any fluctuations early on and address them promptly.
Last but not least: stress management. Stress can wreak havoc on your blood sugar levels so learning techniques like meditation or deep breathing exercises can be beneficial.
Remember:
- Maintain a balanced diet
- Exercise regularly
- Monitor blood glucose levels frequently
- Manage stress effectively
Taking these steps towards a healthier lifestyle won't just manage your diabetes - they'll improve your overall quality of life too.
Knowledge is power when dealing with diabetes. The more informed we are about this condition, the better prepared we are to combat it head-on and live fulfilling lives despite its challenges.
Research, Resources, and Studies:
https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-management/art-20047963
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.