Medically Reviewed by:Scientific Advisory Board
We've all heard about diabetes and eating disorders separately, but what happens when these two health issues intersect? Diabetes Eating Disorders, also known as 'diabulimia', is a condition that's been gaining attention in recent years. It refers to the deliberate misuse of insulin by people with type 1 diabetes for the purpose of weight loss.
It's a disturbing trend we're seeing more frequently among those battling diabetes. Misusing insulin isn't just harmful; it can lead to disastrous health consequences including kidney failure, severe dehydration, and even death. Yet, despite the serious risks associated with this behavior, many people aren't aware of its existence.
Understanding diabulimia starts with getting a grasp on both diabetes and eating disorders independently before looking at how they intertwine. We'll explore each aspect in depth, shedding some light on this often overlooked issue that affects thousands of individuals worldwide.
Understanding Diabetes Eating Disorders
We're diving deep into the complex matter of diabetes eating disorders (DEDs), a critical topic many people aren't aware of. DEDs, as they're known, are unique conditions that affect individuals with Type 1 or Type 2 diabetes. These disorders stem from the complicated relationship between food, body image, and blood sugar control.
People with diabetes need to manage their diet carefully to maintain healthy blood glucose levels. This focus on food can sometimes spiral out of control and lead to unhealthy behaviors such as skipping insulin doses to lose weight or overeating due to fear of hypoglycemia.
If we dig deeper into why this happens, we'll notice that managing diabetes requires constant attention—monitoring blood sugar levels, calculating insulin dosages, resisting certain foods—and it's no surprise that this might trigger anxiety around food.
Here are some common warning signs of DEDs:
- Rapid changes in weight not linked to changes in insulin
- Frequent episodes of hypoglycemia or hyperglycemia
- Fearful or avoidant behavior related to food
It's important that if you identify any of these signs in yourself or someone else with diabetes, you seek help immediately from a healthcare professional who is knowledgeable about both diabetes and eating disorders. Remember: knowledge is power. By understanding more about DEDs and recognizing the signs early on, we can take steps towards prevention and effective treatment.
Effects of Eating Disorders on Diabetic Patients
Eating disorders can have a severe impact on the health and well-being of individuals with diabetes. This is because, in order to manage their blood sugar levels effectively, diabetic patients must adhere to a carefully balanced diet.
For starters, let's look at a common eating disorder among diabetic patients known as "Diabulimia". In this condition, people with type 1 diabetes intentionally reduce or stop taking their insulin in an effort to lose weight. It's quite alarming that according to the National Eating Disorders Association (NEDA), about 40% of females aged 15-30 with Type 1 Diabetes are estimated to have diabulimia.
| Age Group | Estimated percentage with Diabulimia |
|---|---|
| Female aged 15-30 | Approximately 40% |
Now imagine what happens when these patients manipulate their insulin doses. Insulin deprivation can lead to high blood glucose levels (hyperglycemia) which over time can cause serious complications such as:
- Heart disease
- Kidney damage
- Nerve damage
- Eye problems
On the other hand, there's another side where diabetic patients may develop anorexia or bulimia nervosa. These disorders involve self-imposed starvation or binge-eating followed by purging respectively. Both conditions can lead to erratic blood sugar levels making it harder for those living with diabetes.
To add context here, studies suggest that women with diabetes are nearly two and half times more likely to develop an eating disorder than those without it. So you see, the intersection of diabetes and eating disorders isn't something we should overlook.
There's still so much more we need to explore about this topic and its implications for folks dealing with both diabetes and an eating disorder. Stay tuned as we dig deeper into strategies for managing these dual conditions, and most importantly, remember that seeking professional help is key if you or someone you know is grappling with these challenges. We're in this together.
Managing Diabetes while Battling an Eating Disorder
Striking a balance between managing diabetes and overcoming an eating disorder can feel like walking a tightrope. It's a complex path, often laden with pitfalls that can derail your progress. However, armed with the right knowledge and strategies, we believe it's entirely possible to navigate this journey successfully.
The first hurdle we face is the overlapping nature of these two conditions. Both require careful food monitoring which can quickly morph into obsessive behavior in vulnerable individuals. According to research by the American Diabetes Association, people with diabetes are twice as likely to develop an eating disorder compared to those without diabetes.
| Conditions | Risk Level |
|---|---|
| People With Diabetes | Twice As Likely |
| People Without Diabetes | Normal Risk |
It's important not just to be aware of this risk but also understand why it exists. For some, stringent dietary restrictions associated with diabetes management can lead to unhealthy relationships with food, triggering disorders such as bulimia or binge-eating. In others, the desire for weight loss might prompt skipping insulin doses – a dangerous practice known as diabulimia.
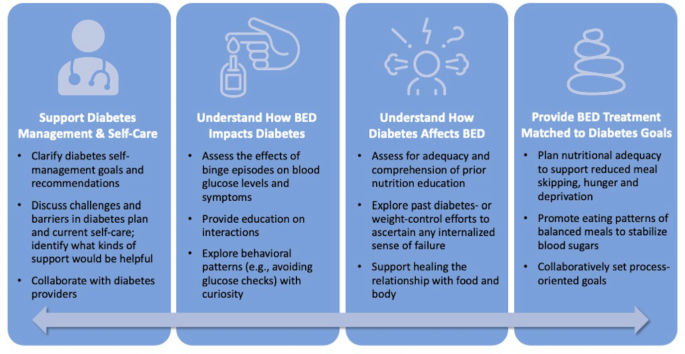
So how do we tackle this tricky terrain? The key lies in implementing tailored strategies that address both conditions simultaneously:
- Establishing Balanced Meal Plans: Collaborate with dietitians who specialize in both diabetes management and eating disorders to create meal plans that keep blood sugar levels stable without promoting disordered eating patterns.
- Therapy and Counseling: Seek out therapists or support groups experienced in dual diagnosis treatment. They provide vital emotional support during this challenging journey.
- Regular Health Checks: Monitoring blood glucose levels regularly ensures you're staying on track health-wise while battling your eating disorder.
Remember: there's no shame in seeking help when you need it. You're not alone in this struggle; thousands of people are grappling with similar challenges every day – and many have come out triumphant on the other side.
Case Studies: Overcoming Diabetes Eating Disorders
We've come across inspiring stories of individuals who overcame diabetes eating disorders. These shining examples can provide hope and motivation to others in similar situations.
One such story is about a woman named Lisa. She's been living with Type 1 diabetes for over 15 years. After being diagnosed, she developed an unhealthy relationship with food due to constant calorie counting and guilt associated with indulgences. However, Lisa took control of her life by seeking professional help from a nutritionist specializing in diabetes management. Through regular counseling sessions, dietary changes, and the support of her family, she managed to overcome her eating disorder while effectively managing her diabetes.
In another instance, we learned about John. He was diagnosed with Type 2 diabetes later in life and struggled with binge eating disorder as a result of the stress associated with his new diagnosis. With the aid of therapy and medication along with lifestyle modifications, he's successfully maintaining stable blood sugar levels now.
The journey wasn't easy for these individuals - it demanded enormous strength, patience, resilience, and consistent effort:
- Professional Help: Both Lisa and John sought help from professionals experienced in treating both diabetes and eating disorders.
- Support System: They leaned on their families for emotional backing during this challenging journey.
- Lifestyle Changes: They incorporated healthy habits into their daily routines - monitoring blood glucose levels regularly, engaging in physical activities they enjoyed, sleeping well.
These case studies illustrate that overcoming an eating disorder while managing diabetes is possible but requires comprehensive care addressing both conditions simultaneously.
We're sharing these examples not just to inspire but also emphasize the importance of recognizing symptoms early on; early intervention can make all the difference. We encourage everyone battling such challenges to seek professional guidance without delay because your health matters.
Conclusion: A Healthy Approach to Diabetes and Eating Disorders
It's crucial for us, as a community, to understand this complex interplay between these two health challenges. So let's summarize our approach towards a healthier lifestyle.
To begin with, we need to recognize the signs that may suggest an eating disorder in someone living with diabetes. These might include unexplained weight loss or gain, constant worrying about body size and shape, or persistent dieting even when it's not medically recommended.
Next, it's imperative that both conditions – diabetes and eating disorders – are treated simultaneously by a team of healthcare professionals who specialize in these areas. This comprehensive approach can increase the chances of successful management and recovery.
For those living with these conditions, self-care is vital. Regular blood glucose monitoring, healthy meal planning, consistent exercise regimens - they all factor into managing diabetes while also addressing an eating disorder.
- Practice mindful eating.
- Create regular exercise schedules.
- Monitor blood sugar levels consistently.
- Seek professional help if needed.
Knowledge is power when dealing with health issues like these. By understanding what we're facing and how best to manage it, we're taking control back from these conditions.
Lastly but importantly - remember you're not alone in your journey. There are numerous resources available; support groups both online and offline can provide comfort during challenging times while offering practical advice from others who've walked similar paths.
Research, Studies and Sources:
https://www.diabetes.org.uk/guide-to-diabetes/life-with-diabetes/diabulimia
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.




