Medically Reviewed by:Scientific Advisory Board
Welcome to our comprehensive guide on eating for a healthy pregnancy, specifically tailored for those grappling with gestational diabetes. Imagine a world where you can navigate through the difficulties of gestational diabetes with ease, understanding the impact of every bite on your blood sugar levels. This guide will help you maintain a nutritious gestational diabetes diet that supports both your wellness and that of your unborn baby.
Short Summary
-
Gestational diabetes can be managed through a healthy diet and lifestyle, including balanced nutrition and low-GI foods.
-
Meal planning strategies help to regulate blood sugar levels, while portion control is essential for overall well-being during pregnancy.
-
Regular monitoring of glucose levels alongside professional guidance can ensure successful management of gestational diabetes.
Understanding Gestational Diabetes and Its Impact on Diet

Embarking on the journey of motherhood, pregnant women often encounter a myriad of challenges. One such hurdle is gestational diabetes, a condition that arises during pregnancy due to hormones from the placenta interfering with the mother’s insulin action. The risk of developing gestational diabetes can lead to complications for both the mother and the unborn child if left untreated.
However, fear not, as a healthy diet and lifestyle can help manage this condition. Consuming nutritious foods and maintaining a balanced diet is crucial to meet increased nutritional needs during pregnancy. But remember, not all healthy foods are created equal — some, like fruit juice, can cause a rapid spike in blood sugar levels and should be avoided.
What is Gestational Diabetes?
Gestational diabetes, a phrase that may sound daunting, is a type of diabetes that occurs during pregnancy. It is caused by hormonal changes that make the body resistant to insulin. This resistance to insulin can lead to elevated blood sugar levels. But how prevalent is this condition? According to the Centers for Disease Control and Prevention, gestational diabetes affects 2-10% of pregnancies annually in the United States.
Insulin, the unsung hero of our bodies, regulates blood sugar levels. Hormonal changes during pregnancy can cause the body to become resistant to insulin. This leads to an increase in high blood sugar levels. This underlines the need to manage gestational diabetes and maintain healthy blood sugar levels.

How Diet Plays a Role
Just as a maestro conducts an orchestra, a nutritious diet orchestrates glucose levels and sustains a healthy weight during pregnancy. However, some foods can hit a sour note. Foods with added sugar, for instance, should be limited as much as possible to prevent spikes in blood sugar levels.
Adhering to a meal plan and consuming a wholesome diet are like the sheet music guiding the maestro — essential components of managing gestational diabetes. And just as the maestro must understand the rhythm and tempo of each piece, one must comprehend the glycaemic index (GI) — a measure that quantifies the rate at which carbohydrates in food affect blood sugar levels post-consumption.
Creating a Balanced Diet for Gestational Diabetes
Crafting a balanced diet for gestational diabetes is akin to creating a masterpiece, with each food item representing a stroke of the brush. By ensuring a healthy range of blood sugar levels, this masterpiece can contribute to a safe and healthy pregnancy. Breakfast, the most important meal of the day, should ideally comprise a combination of whole grains and a protein food.
However, every artist must be mindful of their palette. Just as certain colors may disrupt the harmony of a painting, certain foods like sweets and desserts can lead to elevated blood sugar levels. Portion sizes, too, play a crucial role. For instance, a sensible serving size of starchy foods, like cooked rice, should be approximately 1 cup per meal.
Choosing Nutrient-Dense Foods
Choosing nutrient-dense foods is like selecting the finest quality paints for your masterpiece. They provide essential vitamins and minerals that are vital for a healthy pregnancy. Whole grains and high-fiber foods, such as whole grain bread and brown rice, are particularly beneficial in maintaining low blood sugar levels.
However, beware of the allure of foods labeled as “diabetic” or “suitable for diabetics”. These foods do not provide any additional health benefits and may still cause fluctuations in blood sugar levels. Moreover, they may result in an upset stomach and are typically more expensive than other options.
Carbohydrate Management
Carbohydrates have a significant impact on blood sugar levels, which makes managing carbohydrate intake crucial when dealing with gestational diabetes. When it comes to fruit, it is recommended to consume one small piece, or half a large piece, or approximately one cup of mixed fruit.
Choosing carbohydrates with a lower glycemic index can be beneficial in managing blood sugar levels. But remember, just like a melody that soars too high can become strident, indulging in sweets and desserts can elevate blood sugar levels beyond an acceptable level.
Incorporating Low-GI Foods
Incorporating low-glycemic index (GI) foods into your diet can be likened to introducing harmonious chords into a piece of music. Foods with a GI of 55 or less, like most fruits and non-starchy vegetables, whole or minimally processed grains, beans, pasta, low-fat dairy products, and nuts, are considered low-GI foods.
However, not all low-GI foods are nutritionally beneficial. Just as a musician must be discerning when selecting chords to maintain harmony, you should make a mindful decision when selecting low-GI foods, reading food labels carefully.
Meal Planning and Snacking Strategies
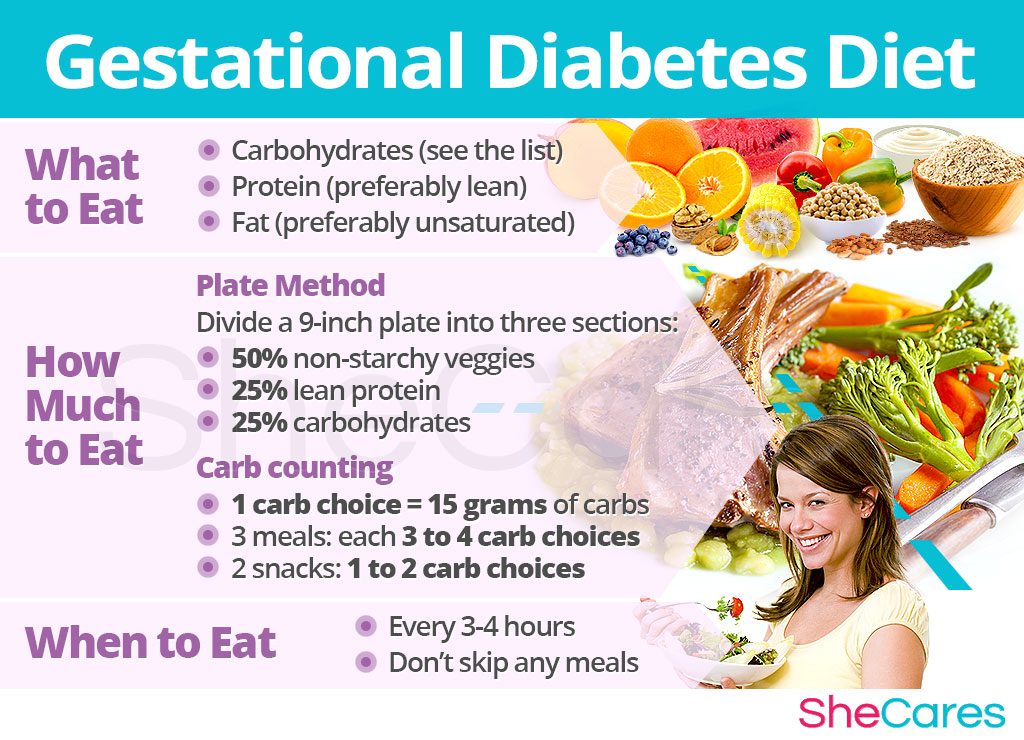
Meal planning and snacking strategies are the rhythm and timing that keep your blood sugar symphony in harmony. Including protein foods and vegetables with each main meal, limiting carbohydrate intake at breakfast to 15-20g, and splitting breakfast into two sittings can be beneficial for gestational diabetes.
Regular monitoring and logging of blood sugar levels at different points during the day can provide insight into the appropriate times to eat, the amount of food to consume, and the types of foods that are most suitable.
Consistent Eating Schedule
Maintaining a consistent eating schedule is like keeping a steady beat. It involves adhering to a similar dietary pattern across different eating situations, consuming the majority of calories earlier in the day, and abstaining from food intake for less than 12 hours per day. It is essential for overall well-being, promoting good digestion, and sustaining a healthy weight.
Splitting breakfast into two sessions can also be beneficial. Like a symphony that begins quietly and builds up to a crescendo, splitting your breakfast can help manage your blood sugar levels more effectively.
Portion Control
Portion control is like controlling the volume of your music. It’s an essential practice in managing the quantity of food consumed at each meal, ensuring that one does not indulge in overeating. This is especially crucial for women with gestational diabetes who need to regulate their blood sugar levels through a balanced and nutritious diet.
Just as a musician uses precise measurements to create the perfect sound, accurate serving sizes can be determined using measuring cups, spoons, or a food scale. Alternatively, one can estimate serving sizes by using their hand as a reference.
Healthy Snack Ideas
Think of healthy snacks as the delightful interludes in your symphony. Choices like cheese sticks, carrots, almonds, Greek yogurt with berries, and hard-boiled eggs can be beneficial for managing blood sugar levels.
For those on the go, a sliced apple or pear can make for a quick, nutritious snack, or you can drink fruit juice as an alternative.
Beverages and Gestational Diabetes
Beverages, like the subtle undertones in a piece of music, can have a significant impact on blood sugar levels. They can assist in regulating glucose levels. However, not all beverages play a harmonious tune. Fruit juice and other fruit juices with added sugar should be avoided as they can disrupt the symphony of a balanced diet.
Sugar alcohols, often found in sugar-free foods, can have the same quantity of carbohydrates as regular sugar and should be closely monitored on food labels, especially when consuming carbohydrate foods.
Avoiding Sugary Drinks
Just as a musician would avoid discordant notes, sugary drinks should be avoided when managing gestational diabetes. These beverages, containing added sugars like soda, fruit juice, sports drinks, energy drinks, and sweetened coffee or tea, can disrupt the harmony of blood sugar levels.
Healthier alternatives, like water, unsweetened tea, and sparkling water, can play a harmonious tune in your dietary symphony.
Hydration and Water Intake
Hydration and water intake play a fundamental role in your symphony of health. They are essential to sustain normal bodily functions during pregnancy and to avoid any potential pregnancy complications.
Drinking 8-12 glasses of water per day is advised during pregnancy to avoid dehydration and avert potential complications.
Lifestyle Factors and Gestational Diabetes Management
In addition to diet, other lifestyle factors also play a significant role in the symphony of managing gestational diabetes. Regular health care visits, exercise, and monitoring of glucose levels are essential components of a gestational diabetes treatment plan.
The initial step in the gestational diabetes treatment plan is akin to the first note in a symphony — ascertaining one’s blood sugar level and ensuring it remains within the desired range.
Exercise and Physical Activity
Like the rhythmic beat that drives a piece of music, regular exercise and physical activity can assist in maintaining blood sugar levels and promoting general well-being during pregnancy. Engaging in both aerobic and resistance exercises at moderate intensity for at least 20-50 minutes twice weekly can be beneficial.
Similar to how a musician warms up before a performance, it’s advisable to start slowly and gradually increase the intensity and duration of exercise.
Monitoring Blood Sugar Levels
Just as a conductor keeps track of each musician in an orchestra, regular monitoring of blood sugar levels is essential in managing gestational diabetes. Blood sugar level monitoring involves the use of a blood glucose meter or a continuous glucose monitor (CGM) to measure the concentration of sugar in a sample of blood, usually taken from the fingertip. Keeping track of your blood sugars can help ensure optimal management of gestational diabetes.
Maintaining a food and activity diary can provide valuable insights into the appropriate times to eat, the amount of food to consume, and the types of foods that are most suitable.
Seeking Professional Guidance
Just as a novice musician seeks guidance from a seasoned maestro, pregnant women dealing with gestational diabetes should seek professional guidance to ensure they are following the optimal diet and lifestyle for their health and their baby’s health. Management of gestational diabetes may entail dietary recommendations, physical activity, blood glucose monitoring, and insulin therapy if necessary.
If one is unable to regulate their glucose levels through diet and exercise alone, it is advisable to discuss this with their healthcare team and consider the potential benefits of taking medication or insulin.
Summary
We’ve explored how each lifestyle aspect — diet, exercise, and regular monitoring of blood sugar levels — contributes to managing gestational diabetes. We’ve seen how adopting a balanced diet, maintaining regular meals and snack schedules, and choosing nutrient-dense foods can keep our health in harmony.
Frequently Asked Questions
What foods to avoid during pregnancy gestational diabetes?
It’s best to avoid sugary drinks and high-GI carbohydrates such as cookies, candy, soft drinks, potatoes, french fries, white rice, and other sweets when managing gestational diabetes.
What is the best food to eat out with gestational diabetes?
When eating out with gestational diabetes, it is best to choose plain dishes such as meat, fish, steamed vegetables, or a plain potato. Additionally, choose broiled meats, fish, and poultry and avoid cream sauces, gravy, and casserole dishes.
Opt for broth-type soups for the best food options.
How many carbs can I eat if I have gestational diabetes?
For gestational diabetes, it is recommended to consume 175 grams of carbohydrates per day or less, and distribute them among three small-to-moderate sized meals and 24 snacks.
This should also be accompanied by monitoring blood sugar levels with a home glucose monitor to determine the effects of food on blood sugar.
Can I eat bananas with gestational diabetes?
You can safely eat bananas with gestational diabetes, as long as you watch your portion size and have it in combination with protein and fiber. Eating 2 to 4 servings of whole fruit per day is recommended, with one serving being 1 medium sized banana.
What is a good diet during pregnancy for gestational diabetes?
To manage gestational diabetes, maintain a well-balanced diet that includes lean proteins, complex carbohydrates, and plenty of non-starchy vegetables. Be sure to limit sugary drinks, fruit juices, and pastries.
Working with a dietitian can help you make the best choices for you and your baby.
References, Studies and Sources:
https://www.ucsfhealth.org/education/dietary-recommendations-for-gestational-diabetes
More About Circufiber.com and Healthcare disclaimer:
Always consult your physician before beginning any program. This general information is not intended to diagnose any medical condition or to replace your healthcare professional. If you experience any pain or difficulty, stop and consult your healthcare provider. Circufiber.com socks are clinically proven to improve micro-circulation in feet and lower extremities in people with Diabetes.
More Author Information:
Dr. Capozzi is a board-certified foot surgeon through the American Board of Foot and Ankle Surgery. He is a Diplomate of the American Academy of Wound Management and Fellow of the American College of Foot and Ankle Surgeons. He completed a three-year residency program in Foot and Ankle Reconstructive Surgery at St. Francis Hospital & Medical Center in Hartford, CT in 2010. Dr. Capozzi is a board-certified Wound Specialist® granted by the American Academy of Wound Management. He is also board-certified in Foot Surgery through the American Board of Foot and Ankle Surgery.




